How to Reduce Impulsivity in an ADHD Child
Learn strategies to reduce impulsivity in children with ADHD. Discover how structure, positive reinforcement, and self-regulation tools can help your child thrive.


Interrupting conversations. Fidgeting. Emotional outbursts. If your child has Attention Deficit Hyperactivity Disorder (ADHD), you may be familiar with these impulsive behaviors. As a parent, it can be challenging to redirect your child's impulsivity. If you're wondering how to reduce impulsivity in ADHD child, these strategies can give your child the tools they need to thrive.
Key Takeaways
- Strategies like schedules and chore charts add structure to your child's day. This helps your child know what to expect.
- Positive reinforcement encourages appropriate behaviors in your child. Clear, immediate consequences discourage inappropriate behavior.
- If your child's symptoms interfere with their daily life or pose a safety risk, contact a professional immediately.
Impulsivity in ADHD: What’s the connection?
If your child has ADHD, you are not alone. Over seven million children under the age of 18 in the United States have ADHD. The disorder is more common in boys than girls. Sixty percent of children with ADHD have a moderate or severe form of the disorder.
Children with ADHD can show a variety of symptoms. The three primary symptoms are impulsivity, hyperactivity, and inattention. Some children with ADHD may have more inattentive behaviors. Other kids may experience more impulsivity and hyperactivity. Your child can also have a combination of inattentive, impulsive, and hyperactive symptoms.
The National Institute of Mental Health defines impulsivity as "acting without thinking or having difficulty with self-control." If your child is impulsive, they may fidget or squirm when sitting. They may run around or climb on furniture at inappropriate times. Your child may have trouble taking turns or waiting in line.
Effective strategies to reduce impulsivity
As a parent, you may wonder how you can help your child with their impulsive behavior. There are many strategies you can use to redirect your child. Over time, you can help them learn to manage or stop their impulsivity.
Every child is different, so there is no "one size fits all" solution. You may need to try several different strategies.
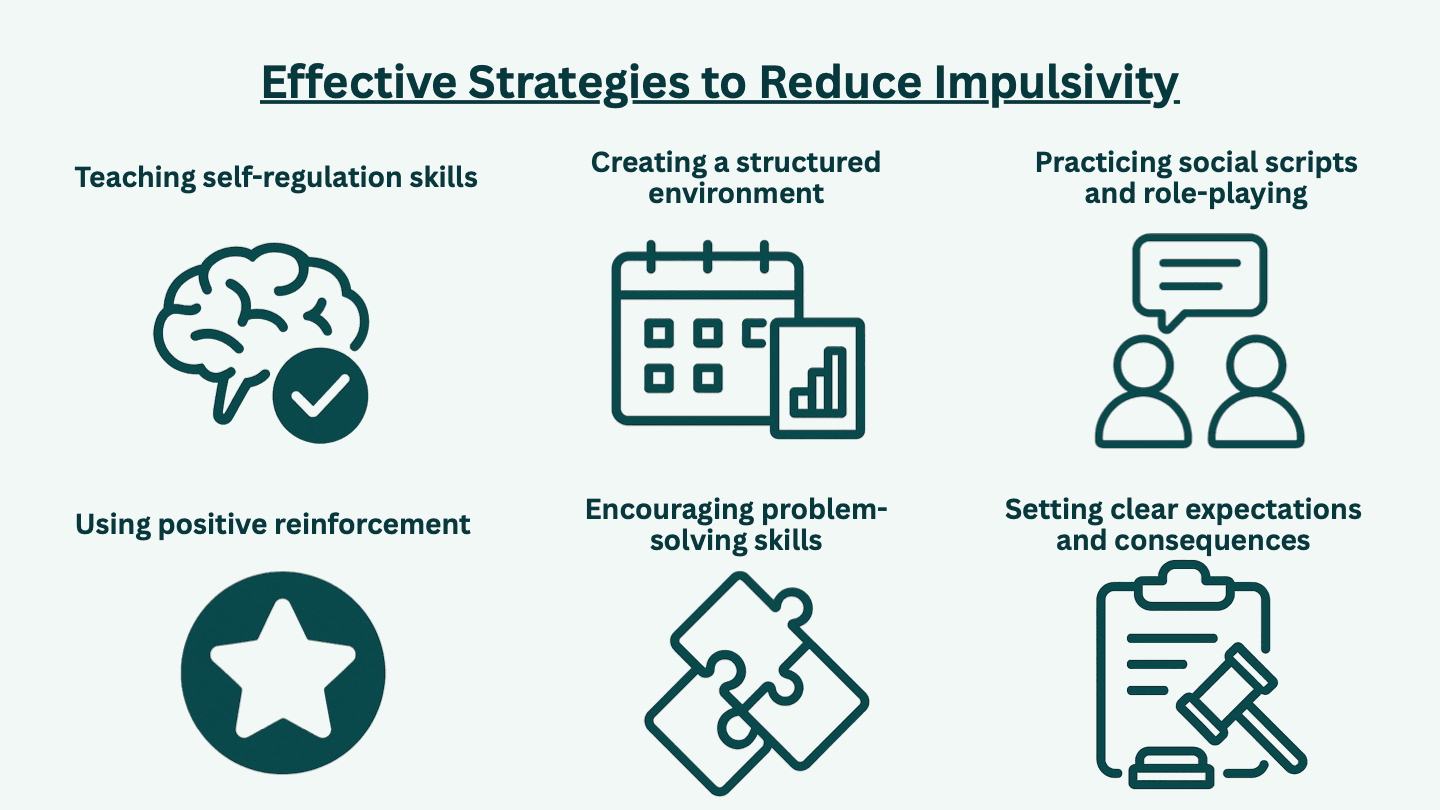
Teaching self-regulation skills
People who can self-regulate can manage their thoughts and feelings. Self-regulation is a skill that your child can develop and practice with your help. To develop this skill, you can start by teaching your child to notice their impulsive behaviors. Once they learn to notice their behavior, they can learn to self-regulate.
As a parent, you can teach your child to self-monitor and self-regulate by providing feedback. When your child acts impulsively, you can ask them to pause and think about what happened. Ask your child if that is really what they want to do. You may ask if they acted without thinking first. You can also ask what they should do now. This helps your child start to self-monitor and self-regulate.
When your child acts impulsively, you may feel frustrated. This is a normal, understandable reaction. Instead of reacting in the moment, you may find it helpful to develop a script for when your child acts out. This script can help you manage your emotions and stay calm.
Like all skills, self-regulation takes practice! At times, there may be setbacks. As a parent, you can help your child by celebrating their wins. Provide positive feedback when they stop, think, and correct their behavior.
Creating a structured environment
All children need structure, but children with ADHD especially benefit from a structured environment. A structured environment helps your child understand what to expect and when. Structure can reduce the impulsivity and anxiety common in kids with ADHD.
A structured environment can include tools like a daily schedule, chore charts, and behavior cards. Keep schedules and charts simple with few words. You can use simple graphics to show the steps in the routine. A picture of a toothbrush can represent brushing their teeth. You can use a picture of a bed to represent bedtime or a book to represent homework.
Set up designated areas in your home for different activities. For example, you can set up a desk for homework or a special armchair for reaching. This can help your child transition from one activity to the next.
Using positive reinforcement
Positive reinforcement is a powerful tool for helping children with ADHD manage their behavior.[8] When your child acts appropriately, you can give them positive feedback. This can be verbal praise or a tangible reward, such as a treat. When you use positive reinforcement after the appropriate behavior, your child is more likely to repeat the behavior.
Positive reinforcement will also help build your child's self-esteem. Many children with ADHD experience more criticism than their neurotypical friends. As a parent, you can be your child's cheerleader. Look for opportunities to praise your child.
Encouraging problem-solving skills
If your child has ADHD, they may rush to solve a problem without stopping to think. As a parent, you can adopt a collaborative style to solving problems. Encourage your child to pause and take a breath. Ask your child how they want to solve the problem. This gives your child a chance to make decisions and build their confidence.
Complex problems may make your child feel overwhelmed or anxious. Your child may struggle with starting large homework assignments. You can help your child break down the project into smaller tasks. Creating to-do lists and schedules can help your child stay on track.
Practicing social scripts and role-playing
If your child has ADHD with impulsivity, they may struggle with taking turns and sharing. Your child may act out when they don't get what they want. You can help your child improve their social skills with scripts and role-playing.
You can start by picking one or two social skills to focus on. If your child has trouble sharing, you can role-play a scenario where your child has to share a favorite toy. You may want to write a script that models how to act. This is a great opportunity for your child to practice self-monitoring and self-regulation.
Setting clear expectations and consequences
There will be times when you need to set rules and expectations for your child. When setting expectations, the rules and consequences should be clear. Rules should be simple and clear. Write down the rules and post them in an area where your child will see them.
When your child breaks a rule, the consequences should be immediate and age-appropriate. Your child should know what to expect if they break a rule. If one consequence is losing screen time, don't give in when your child complains. Be consistent.
When to seek professional support
The above strategies can help your child develop self-control, but these techniques may not be enough. If your child struggles with anxiety or depression as a result of ADHD, you may benefit from professional support.
Sometimes, impulsivity shows up as aggression or risk-taking. If impulsivity presents a safety issue for your child or others, contact a professional for help immediately.
How therapy can help
Therapy can help your child modify their impulsive behaviors. Social skills training can help your child prepare for common situations where they may feel overwhelmed. Play therapy can help your young child practice expressing and regulating their emotions.
Parents can be involved in therapy too for their children. Parent training is a type of therapy for parents. This therapy will give you the tools to strengthen your bond with your child.
Conclusion
Raising a child is a journey with ups and downs, but you can set your child up for success. Create a structured environment with clear rules and expectations. Teach your child to self-regulate their behavior. You don't have to manage your child's impulsivity alone. A professional therapist can give your child the added support they need.
Get support for your child
You aren’t alone. Get mental health support for your child from the comfort of your home with Emora Health. Our evidence-based treatment plans are designed specifically for your child’s needs. We accept most major health plans.